
When Is A Hipaa Authorization Required Compliancehome This authorization serves as a crucial safeguard against unauthorized access to sensitive health data, preventing potential misuse or disclosure without the individual’s knowledge or consent. obtaining hipaa authorization also promotes transparency and informed consent. § 164.508 uses and disclosures for which an authorization is required. (a) standard: authorizations for uses and disclosures — (1) authorization required: general rule.

When Is A Hipaa Authorization Required Compliancehome If informed consent or reconsent (ie., asked to sign a revised consent or another informed consent) is obtained from research subjects after the compliance date, the covered entity must obtain individual authorization as required at 45 cfr 164.508 for the use or disclosure of protected health information once the consent obtained before the. When is hipaa authorization required? 45 cfr §164.508 details the uses and disclosures of phi that require an authorization to be obtained from a patient plan member before information can be shared or used. When is an authorization required by hipaa? an authorization is required when a healthcare provider or a health plan wants to use or disclose a patient's phi for purposes that are not related to treatment, payment, or healthcare operations. The hipaa privacy rules generally prohibit healthcare providers and their business associates from using or disclosing protected health information (“phi”) unless (1) they have a valid written hipaa authorization signed by the patient or the patient’s personal representative, or (2) a specific regulatory exception applies. 1 many if not most authorizations received by providers are.

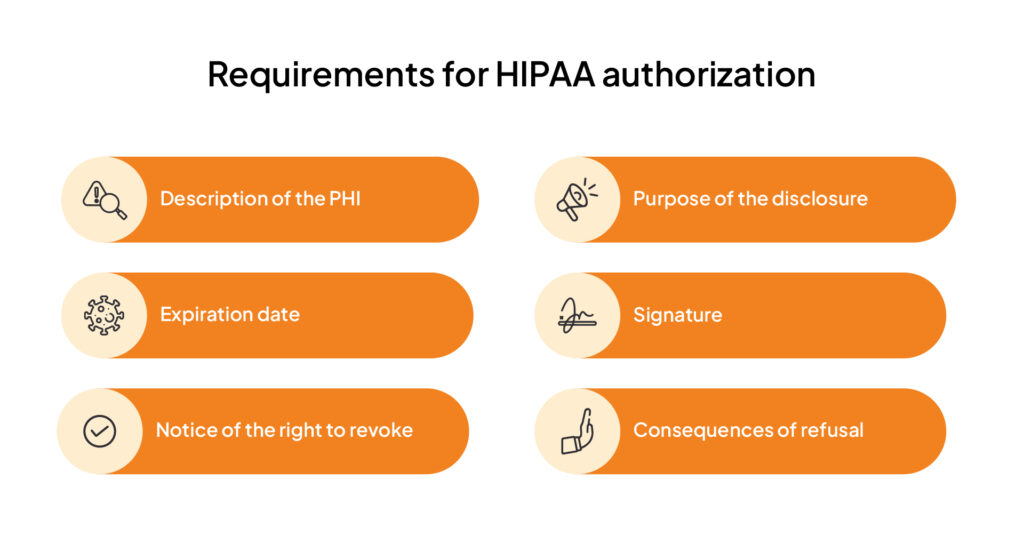
When Is A Hipaa Authorization Required Compliancehome When is an authorization required by hipaa? an authorization is required when a healthcare provider or a health plan wants to use or disclose a patient's phi for purposes that are not related to treatment, payment, or healthcare operations. The hipaa privacy rules generally prohibit healthcare providers and their business associates from using or disclosing protected health information (“phi”) unless (1) they have a valid written hipaa authorization signed by the patient or the patient’s personal representative, or (2) a specific regulatory exception applies. 1 many if not most authorizations received by providers are. A hipaa authorization is a document detailing, in full, the precise uses and disclosures of phi. when a person signs an authorization, he she is agreeing to have his her medical data used or disclosed in ways stated on the authorization. Review hipaa authorization basics learn when to obtain one from a patient, and how to respond if you receive one asking you for a patient's phi.

A Hipaa Authorization Has Which Of The Following Characteristics A hipaa authorization is a document detailing, in full, the precise uses and disclosures of phi. when a person signs an authorization, he she is agreeing to have his her medical data used or disclosed in ways stated on the authorization. Review hipaa authorization basics learn when to obtain one from a patient, and how to respond if you receive one asking you for a patient's phi.
Hipaa Authorization Find Out Why Is It Required Sprinto